New treatment could help improve outcome for prostate cancer sufferers
Researchers at Queen's University in Belfast have developed a new treatment to be used in combination with radiotherapy that could significantly improve treatment outcomes for men with locally advanced prostate cancer.
The treatment can make cancerous cells up to 30% more receptive to radiotherapy while simultaneously reducing adverse side-effects that limit quality of life.
Radiotherapy is extensively used to treat various localised cancers including prostate cancer, offering the best chance for curative intervention.
However, approximately 30% of prostate cancer patients experience treatment failure leading to disease progression.
The research team at Queen's has developed a new nanomedicine comprised of tiny gold particles, coated in a small peptide called RALA.
If these nanoparticles are present in tumour cells when treated with radiotherapy, they increase the cell-killing potential of this conventional treatment, helping to reduce the risk of disease relapse.
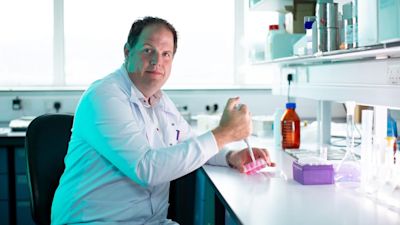
Professor Helen McCarthy, from the School of Pharmacy at Queen's University, said: "The peptide enables the gold nanoparticles to be delivered more efficiently to the tumour cells.
"The gold then interacts with the radiotherapy, increasing the cell-killing effect in a highly localised manner."
Dr Jonathan Coulter said: "Our research has shown that ultra-low concentrations of the RALA-gold nanoparticles effectively sensitise prostate tumour cells to radiotherapy.
"Now we want to build on this work, to address the second major challenge, consistently delivering sufficient nanoparticles to the tumour throughout a patient's radiotherapy.
"We are delighted that Prostate Cancer UK are supporting our proposal to develop a biodegradable implant designed to provide sustained release of the gold nanoparticles.
"Following insertion into the main tumour lesion, the biodegradable implant will consistently release the nanoparticles over time. This is opposed to current approaches that involve daily injections.
"Following consultation with a local prostate cancer patient focus group, we learned that a one-off implant would be better tolerated by patients than regular injections to the tumour."
The multi-disciplinary team has recently been awarded #376,000 from Prostate Cancer UK to evaluate the effectiveness of these implants at increasing the sensitivity of prostate cancer cells to radiotherapy.